Bidirectional two-sample mendelian randomization investigation of the causal association between chronic kidney disease and renal function related indicators with insomnia
-
摘要:
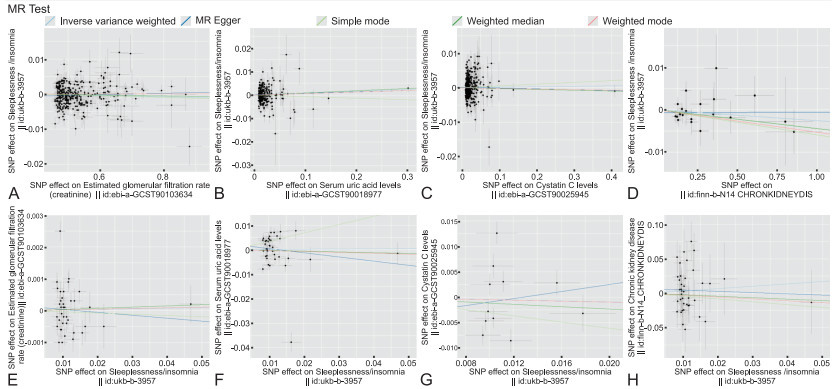
目的 慢性肾脏病(CKD)及肾功能相关指标异常与失眠在临床上常同时发病,本研究旨在通过双向两样本孟德尔随机化(MR)方法探讨其潜在因果关联。 方法 从已公开发表、欧洲人群的全基因组关联研究数据集中筛选出与暴露因素强相关且满足连锁不平衡条件的单核苷酸多态性(SNPs)作为工具变量,并从相应结局中提取SNPs行MR分析。以逆方差加权法(IVW)作为主要因果推断结果,以MR-Egger回归、加权中值、加权众数、简单众数法作为IVW的补充与验证。 结果 IVW法提示CKD及血清肌酐、血尿酸、胱抑素C与失眠之间不存在显著因果关联,其OR(95% CI)分别为0.997(0.993~1.002)、0.924(0.844~1.011)、1.008(0.997~1.019)、1.001(0.993~1.009),均P>0.05;失眠对CKD及血清肌酐、血尿酸、胱抑素C亦不存在显著因果关联,OR(95% CI)分别为1.403(0.625~3.151)、1.002(0.983~1.021)、1.010(0.871~1.170)、0.954(0.679~1.342),均P>0.05;MR-Egger回归法、加权中值方法、加权众数法、简单众数法均进一步验证CKD及血清肌酐、血清尿酸、胱抑素C与失眠之间不存在双向因果关联。此外,水平多效性检验、异质性检验、留一法分析结果总体效应不受单个工具变量的影响,进一步佐证MR分析结果稳健可靠。 结论 CKD及肾功能相关指标与失眠不存在明显双向因果关联。 Abstract:Objective Chronic kidney disease (CKD) and renal function-related index abnormalities and insomnia often occur simultaneously in clinical practice. This study aimed to explore the potential causal association through Bidirectional two-sample Mendelian randomization (MR) analysis. Methods Single nucleotide polymorphisms (SNPs) that were strongly correlated with exposure factors and satisfied the linkage disequilibrium were screened from the published genome-wide association study (GWAS) dataset of European population as instrumental variables, and the SNPs were extracted from the corresponding outcomes for MR analysis. The inverse-variance weighted (IVW) method was used as the main causal inference result, and MR-Egger regression, weighted median, weighted mode, and simple mode methods were used as supplements and validation of IVW to explore the two-way causal association between chronic kidney disease and its related indicators and insomnia. Results There was no significant causal association between CKD, serum creatinine, serum uric acid, cystatin C and insomnia by IVW method. The OR (95% CI) were 0.997 (0.993-1.002), 0.924 (0.844-1.011), 1.008 (0.997-1.019), 1.001 (0.993-1.009), respectively (P>0.05). There was no significant causal association between insomnia and CKD and serum creatinine, serum uric acid, and cystatin C. The OR (95% CI) were 1.403 (0.625~3.151), 1.002 (0.983-1.021), 1.010 (0.871-1.170), and 0.954 (0.679-1.342), respectively (P>0.05). MR-Egger regression method, weighted median method, weighted mode method, and simple mode method further verified that there was no bidirectional causal relationship between CKD and its related indicators (serum creatinine, serum uric acid, cystatin C) and insomnia (P>0.05). In addition, the overall effect of level pleiotropy test, heterogeneity test, and leave one method analysis results were not affected by a single instrumental variable, further confirming the robustness and reliability of MR analysis results. Conclusion There is no obvious bidirectional causal association between CKD and renal function related indicators and insomnia. -
Key words:
- Chronic kidney disease /
- Renal function /
- Insomnia /
- Mendelian randomization analysis
-
表 1 CKD及其相关指标(Cr、UA、Cys-C)与失眠的正向与反向MR分析
Table 1. Forward and reverse MR analysis of CKD and its related indicators (Cr, UA, Cys-C) with insomnia
MR 暴露 OR值(95% CI) P值 结局 OR值(95% CI) P值 MR-Egger CKD 1.000(0.991~1.009) 0.990 CKD 0.835(0.075~9.272) 0.884 Weighted median 0.996(0.989~1.002) 0.204 0.810(0.252~2.598) 0.722 IVW 0.997(0.993~1.002) 0.295 1.403(0.625~3.151) 0.412 Simple mode 0.994(0.982~1.006) 0.348 0.663(0.077~5.713) 0.710 Weighted mode 0.995(0.985~1.004) 0.300 0.762(0.166~3.500) 0.729 MR-Egger Cr 1.084(0.888~1.325) 0.428 Cr 0.991(0.933~1.053) 0.767 Weighted median 0.949(0.853~1.055) 0.332 1.004(0.988~1.020) 0.654 IVW 0.924(0.844~1.011) 0.085 1.002(0.983~1.021) 0.858 Simple mode 0.907(0.687~1.197) 0.491 0.996(0.960~1.033) 0.835 Weighted mode 1.010(0.869~1.174) 0.897 1.002(0.979~1.026) 0.858 MR-Egger UA 1.006(0.991~1.021) 0.427 UA 0.843(0.510~1.392) 0.509 Weighted median 1.009(0.999~1.020) 0.089 0.969(0.866~1.084) 0.585 IVW 1.008(0.997~1.019) 0.164 1.010(0.871~1.170) 0.897 Simple mode 0.993(0.955~1.034) 0.749 1.407(1.006~1.967) 0.053 Weighted mode 1.007(0.997~1.017) 0.203 0.964(0.799~1.162) 0.699 MR-Egger Cys-C 0.998(0.987~1.009) 0.675 Cys-C 1.413(0.192~10.388) 0.742 Weighted median 0.998(0.989~1.006) 0.600 0.889(0.710~1.114) 0.306 IVW 1.001(0.993~1.009) 0.755 0.954(0.679~1.342) 0.789 Simple mode 1.005(0.974~1.037) 0.747 0.737(0.437~1.243) 0.279 Weighted mode 0.998(0.990~1.006) 0.664 0.953(0.619~1.466) 0.830 表 2 CKD及其相关指标(Cr、UA、Cys-C)与失眠的正向与反向敏感性分析
Table 2. Forward and reverse sensitivity analysis of CKD and its related indicators (Cr, UA, Cys-C) with insomnia
暴露 水平多效性 异质性 结局 水平多效性 异质性 MR-Egger回归截距 P值 Cochran' s Q检验 P值 MR-Egger回归截距 P值 Cochran' s Q检验 P值 CKD -0.001 0.519 16.924 0.595 CKD 0.006 0.656 46.525 0.162 Cr -0.001 0.080 742.670 <0.001 Cr 0 0.710 182.112 <0.001 UA <0.001 0.720 513.333 <0.001 UA 0.002 0.465 241.867 <0.001 Cys-C 0 0.340 722.209 <0.001 Cys-C -0.004 0.704 84.076 <0.001 -
[1] 汤曦, 石运莹, 王俭勤, 等. 中国成人慢性肾脏病及其并发症早期筛查临床路径专家建议(2023版)[J]. 中国实用内科杂志, 2023, 43(3): 198-205.TANG X, SHI Y Y, WANG J Q, et al. Expert recommendations on the early screening path of adult chronic kidney disease and its complications in China(2023 edition)[J]. Chinese Journal of Practical Internal Medicine, 2023, 43(3): 198-205. [2] HAN Y Y, SONG X Y, LIU Y, et al. The effects of depression and age on sleep disturbances in patients with non-dialysis stage 3-5 chronic kidney disease: a single-center study[J]. Int Urol Nephrol, 2020, 52(4): 739-748. doi: 10.1007/s11255-020-02416-y [3] LYONS O D. Sleep disorders in chronic kidney disease[J]. Nat Rev Nephrol, 2024, 20(10): 690-700. doi: 10.1038/s41581-024-00848-8 [4] 施小燕, 时宗泽, 张富亿, 等. 慢性肾脏病睡眠障碍的中医外治技术研究进展[J]. 中国医学创新, 2024, 21(13): 158-162.SHI X Y, SHI Z Z, ZHANG F Y, et al. Research progress on external treatment techniques of Traditional Chinese Medicine for sleep disorders in chronic kidney disease[J]. Medical Innovation of China, 2024, 21(13): 158-162. [5] 于天琦, 徐文涛, 苏雅娜, 等. 孟德尔随机化研究基本原理、方法和局限性[J]. 中国循证医学杂志, 2021, 21(10): 1227-1234.YU T Q, XU W T, SU Y N, et al. Mendelian randomization: the basic principles, methods and limitations[J]. Chinese Journal of Evidence-based Medicine, 2021, 21(10): 1227-1234. [6] TAN L H, CHEN P S, CHING H Y, et al. Insomnia and poor sleep in CKD: a systematic review and meta-analysis[J]. Kidney Med, 2022, 4(5): 100458. DOI: 10.1016/j.xkme.2022.100458. [7] 李桦, 钟禹文, 罗浩, 等. 不良生活方式与慢性肾脏疾病的孟德尔随机化研究[J]. 现代预防医学, 2024, 51(15): 2808-2812, 2823.LI H, ZHONG Y W, LUO H, et al. Mendelian randomization study on unhealthy lifestyle and chronic kidney disease[J]. Modern Preventive Medicine, 2024, 51(15): 2808-2812, 2823. [8] RICARDO A C, KNUTSON K, CHEN J S, et al. The association of sleep duration and quality with CKD progression[J]. J Am Soc Nephrol, 2017, 28(12): 3708-3715. doi: 10.1681/ASN.2016121288 [9] 王宜飞, 孙倩, 夏中元. 昼夜节律、时钟基因与慢性肾脏病发病关系的研究进展[J]. 山东医药, 2021, 61(32): 81-85.WANG Y F, SUN Q, XIA Z Y. Research progress on the relationship between circadian rhythm, clock genes and the onset of chronic kidney disease[J]. Shandong Medical Journal, 2021, 61(32): 81-85. [10] ZHANG H J, WANG B, CHEN C, et al. Sleep patterns, genetic susceptibility, and incident chronic kidney disease: a prospective study of 370 671 participants[J]. Front Neurosci, 2022, 16: 725478. DOI: 10.3389/fnins.2022.725478. [11] 陈泽平, 马华林. 睡眠时间对慢性肾脏病的影响及其机制的研究进展[J]. 内科, 2023, 18(5): 461-469.CHEN Z P, MA H L. Research progress on the impact of sleep duration on chronic kidney disease and its mechanism[J]. Internal Medicine, 2023, 18(5): 461-469. [12] 张颖煜. "益肾清利泄浊方"延缓慢性肾脏病3-5期肾功能进展的临床疗效观察[D]. 南京: 南京中医药大学, 2022.ZHANG Y Y. Clinical efficacy observation of "Yishen Qingli Xiezhuo Prescription" in delaying the progression of renal function in chronic kidney disease stage 3-5[D]. Nanjing: Nanjing University of Chinese Medicine, 2022. [13] 邓祖抚. 慢性肾脏病患者肾功能分期、血清胱抑素C及生命质量与睡眠呼吸障碍的相关性研究[J]. 世界睡眠医学杂志, 2022, 9(4): 633-635.DENG Z F. Study on the correlation between renal function stage, serum cystatin C, quality of life and sleep disordered breathing in patients with chronic kidney disease[J]. World Journal of Sleep Medicine, 2022, 9(4): 633-635. [14] 朱永福, 林崇泽, 邵思思. 高尿酸血症相关肾损害的危险因素分析[J]. 浙江临床医学, 2024, 26(5): 700-702.ZHU Y F, LIN C Z, SHAO S S. Analysis of risk factors for renal damage associated with hyperuricemia[J]. Zhejiang Clinical Medical Journal, 2024, 26(5): 700-702. [15] 胡艳, 陶敏, 潘星, 等. 慢性肾脏病人群中高尿酸血症的患病率及危险因素研究[J]. 中华全科医学, 2020, 18(12): 1989-1993. doi: 10.16766/j.cnki.issn.1674-4152.001670HU Y, TAO M, PAN X, et al. Prevalence and risk factors of hyperuricemia in patients with chronic kidney disease[J]. Chinese Journal of General Practice, 2020, 18(12): 1989-1993. doi: 10.16766/j.cnki.issn.1674-4152.001670 [16] 蔡银香, 杨雪球, 姜俊, 等. 慢性肾脏病患者睡眠障碍的相关因素分析[J]. 安徽医科大学学报, 2024, 59(3): 521-526.CAI Y X, YANG X Q, JIANG J, et al. Analysis of factors related to sleep disorders in patients with chronic kidney disease[J]. Acta Universitatis Medicinalis Anhui, 2024, 59(3): 521-526. [17] PRABHAKAR N R, PENG Y J, NANDURI J. Hypoxia-inducible factors and obstructive sleep apnea[J]. J Clin Invest, 2020, 130(10): 5042-5051. doi: 10.1172/JCI137560 [18] 卢春宇, 成水芹, 王金泉. 昼夜节律紊乱对慢性肾脏病的影响[J]. 肾脏病与透析肾移植杂志, 2023, 32(3): 265-269.LU C Y, CHENG S Q, WANG J Q. Circadian rhythm disorder in chronic kidney disease[J]. Chinese Journal of Nephrology, Dialysis & Transplantation, 2023, 32(3): 265-269. [19] VIGOUREUX T F D, LEE S, BUXTON O M, et al. Stressor reactivity to insufficient sleep and its association with body mass index in middle-aged workers[J]. J Sleep Res, 2020, 29(6): e12955. DOI: 10.1111/jsr.12955. [20] MANOLIS T A, MANOLIS A A, APOSTOLOPOULOS E J, et al. Cardiovascular complications of sleep disorders: a better night ' s sleep for a healthier heart/from bench to bedside[J]. Curr Vasc Pharmacol, 2021, 19(2): 210-232. [21] SCHIPPER S B J, VAN VEEN M M, ELDERS P J M, et al. Sleep disorders in people with type 2 diabetes and associated health outcomes: a review of the literature[J]. Diabetologia, 2021, 64(11): 2367-2377. doi: 10.1007/s00125-021-05541-0 [22] LI K X, ZHAO J X, YANG W J, et al. Sleep traits and risk of end-stage renal disease: a Mendelian randomization study[J]. BMC Medical Genomics, 2023, 16(1): 76. DOI: 10.1186/s12920-023-01497-9. -





 下载:
下载: