Risk factors and predictive model construction of post-traumatic stress disorder in patients with traumatic brain injury
-
摘要:
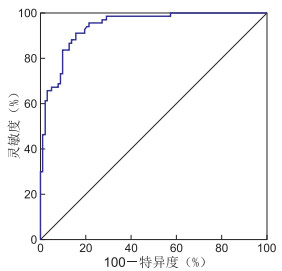
目的 分析颅脑损伤患者发生创伤后应激障碍的危险因素并构建风险预测模型,为早期识别及预防创伤后应激障碍发生提供理论依据。 方法 便利抽样法选择2022年4月—2024年2月阜阳市第五人民医院神经外科住院的170例颅脑损伤患者为研究对象,根据出院后1个月患者是否发生创伤后应激障碍分为应激障碍组(67例)和无应激障碍组(103例)。采用二分类logistic回归模型分析创伤后应激障碍的危险因素并构建风险预测模型,通过ROC曲线检验预测效能。 结果 颅脑损伤患者创伤后应激障碍发生率为39.41%(67/170)。女性(OR=4.509,P=0.009)、有后遗症(OR=3.868,P=0.040)、失眠(OR=2.537,P=0.007)均是创伤后应激障碍发生的危险因素,有赔偿/报销(OR=0.282,P=0.031)、创伤后成长水平高(OR=0.840,P<0.001)、社会关系质量良好(OR=0.913,P=0.017)均是创伤后应激障碍发生的保护因素。Hosmer-Lemeshow拟合优度检验结果(χ2=4.314,P=0.828)说明回归模型匹配度良好,ROC曲线下面积为0.942(95% CI:0.909~0.974,P<0.001),灵敏度及特异度分别为91.0%和84.5%。 结论 颅脑损伤患者创伤后应激障碍发生率偏高,女性、无赔偿/报销、有后遗症、睡眠不足、创伤性成长水平低及社会关系质量差等危险因素会增加创伤后应激障碍的发生风险,建立的风险预测模型具有良好的预测性,可为患者创伤后应激障碍临床评估和早期干预提供理论依据。 Abstract:Objective The risk factors of post-traumatic stress disorder in patients with craniocerebral injury were analyzed and a risk prediction model was constructed to provide a theoretical basis for early identification and prevention of post-traumatic stress disorder. Methods A total of 170 patients with craniocerebral injury who were hospitalized in the Department of Neurosurgery of the Fifth People ' s Hospital of Fuyang City from April 2022 to February 2024 were selected as the study objects by convenient sampling method. According to whether the patients developed PTSD one month after discharge, they were divided into a stress disorder group (n=67) and a no-stress disorder group (n=103). The binary logistic regression model was used to analyze the risk factors of PTSD and to construct a risk prediction model. The predictive efficacy was tested by the ROC curve. Results The incidence of post-traumatic stress disorder in traumatic brain injury patients was 39.41% (67/170). Female (OR=4.509, P=0.009), sequelae (OR=3.868, P=0.040), insomnia (OR=2.537, P=0.007) were risk factors for the occurrence of post-traumatic stress disorder, and there was compensation/reimbursement (OR=0.282, P=0.031), high level of post-traumatic growth (OR=0.840, P < 0.001) and good quality of social relations (OR=0.913, P=0.017) were the protective factors for the occurrence of post-traumatic stress disorder. Hosmer-Lemeshow goodness of fit test results (χ2=4.314, P=0.828) indicated that the regression model had a good match, and the AUC was 0.942 (95% CI: 0.909-0.974, P < 0.001), sensitivity and specificity were 91.0% and 84.5%. Conclusion There is a high incidence of post-traumatic stress disorder in patients with head injuries. Female, no compensation/reimbursement, sequelae, lack of sleep, low level of traumatic growth, poor quality of social relations, and other risk factors will increase the risk of post-traumatic stress disorder. The established risk prediction model has a good prediction, providing a theoretical basis for clinical assessment and early intervention of patients with post-traumatic stress disorder. -
表 1 TBI患者PTSD发生的单因素分析
Table 1. Univariate analysis of PTSD in TBI patients
项目 无PTSD组(n=103) PTSD组(n=67) 统计量 P值 性别[例(%)] 13.867a <0.001 男性 74(71.84) 29(43.28) 女性 29(28.16) 38(56.72) 年龄(x±s, 岁) 50.86±16.15 56.64±12.65 2.475b 0.014 学历[例(%)] 0.051a 0.975 初中及以下 45(43.69) 30(44.78) 高中或中专 35(33.98) 23(34.33) 大专及以上 23(22.33) 14(20.89) 家庭月收入[例(%)] 1.851a 0.396 <5 000元 21(20.39) 13(19.40) 5 000~8 000元 42(40.78) 34(50.75) >8 000元 40(38.83) 20(29.85) 婚姻状态[例(%)] 6.466a 0.011 已婚 91(88.35) 49(73.13) 未婚/离异/丧偶 12(11.65) 18(26.87) 有无赔偿/报销[例(%)] 13.500a <0.001 无 35(33.98) 42(62.69) 有 68(66.02) 25(37.31) 主要照顾者[例(%)] 0.410a 0.815 配偶 51(49.51) 31(46.27) 子女 33(32.04) 21(31.34) 其他 19(18.45) 15(22.39) 入院时GCS评分[例(%)] 11.323a 0.003 ≤8分 7(6.80) 16(23.88) 9~12分 36(34.95) 24(35.82) 13~15分 60(58.25) 27(40.30) 有无后遗症[例(%)] 20.717a <0.001 无 94(91.26) 42(62.69) 有 9(8.74) 25(37.31) 住院时间[例(%)] 4.406a 0.036 ≤10 d 60(58.25) 28(41.79) >10 d 43(41.75) 39(58.21) 损伤到诊治时间[例(%)] 4.776a 0.029 ≤6 h 83(80.58) 44(65.67) >6 h 20(19.42) 23(34.33) 损伤原因[例(%)] 1.185a 0.757 车祸伤 33(32.04) 23(34.33) 坠落伤 32(31.07) 16(23.88) 摔伤 26(25.24) 18(26.87) 其他 12(11.65) 10(14.92) 损伤类型[例(%)] 0.259a 0.611 开放性 33(32.04) 19(28.36) 闭合性 70(67.96) 48(71.64) 睡眠质量[例(%)] 28.331a <0.001 无睡眠障碍 59(57.28) 15(22.39) 可疑失眠 32(31.07) 23(34.33) 失眠 12(11.65) 29(43.28) PTGI得分(x±s, 分) 77.41±8.52 65.25±6.87 9.783b <0.001 SRQS得分(x±s, 分) 54.13±7.47 47.30±6.74 6.047b <0.001 注:a为χ2值,b为t值。 表 2 TBI患者PTSD发生危险因素的自变量赋值
Table 2. Assignment of independent variables for PTSD risk factors in TBI patients
变量 赋值方法 性别 男性=1,女性=2 年龄 连续性变量,以实际值赋值 婚姻状态 已婚=0,未婚/离异/丧偶=1 有无赔偿/报销 有=1,无=0 入院时GCS评分 ≤8分=1,9~12分=2,13~15分=3 有无后遗症 有=1,无=0 住院时间 ≤10 d=1,>10 d=2 损伤到诊治时间 ≤6 h=1,>6 h=2 睡眠质量 无睡眠障碍=(0,0),可疑失眠=(1,0),失眠=(0,1) PTGI得分 连续性变量,以实际值赋值 SRQS得分 连续性变量,以实际值赋值 表 3 TBI患者PTSD发生的危险因素分析
Table 3. Analysis of risk factors for PTSD in TBI patients
变量 B SE Waldχ2 P值 OR值 95% CI 性别 1.506 0.580 6.735 0.009 4.509 1.446~14.063 年龄 0.027 0.019 2.003 0.157 1.027 0.990~1.065 婚姻状态 0.417 0.809 0.266 0.606 1.518 0.311~7.411 有赔偿/报销 -1.266 0.586 4.668 0.031 0.282 0.089~0.889 入院时GCS评分 -0.286 0.387 0.544 0.461 0.752 0.352~1.606 有后遗症 1.353 0.660 4.199 0.040 3.868 1.061~14.109 住院时间 0.763 0.573 1.775 0.183 2.145 0.698~6.589 损伤到诊治时间 0.490 0.630 0.605 0.437 1.632 0.475~5.613 睡眠质量 0.931 0.342 7.402 0.007 2.537 1.297~4.963 PTGI得分 -0.174 0.038 21.281 <0.001 0.840 0.780~0.905 SRQS得分 -0.091 0.038 5.724 0.017 0.913 0.848~0.984 -
[1] SHEN L B, HUANG Y X, LIAO Y J, et al. Effect of high-frequency repetitive transcranial magnetic stimulation over M1 for consciousness recovery after traumatic brain injury[J]. Brain Behav, 2023, 13(5): e2971. DOI: 10.1002/brb3.2971. [2] 罗建, 许兆军. 血浆B型利钠肽与颅脑损伤严重程度的关系及对脑心综合征的预测价值[J]. 中华全科医学, 2022, 20(2): 233-236. doi: 10.16766/j.cnki.issn.1674-4152.002320LUO J, XU Z J. Relationship between plasma B-type natriuretic peptide and severity of craniocerebral injury and its predictive effect on cerebral heart syndrome[J]. Chinese Journal of General Practice, 2022, 20(2): 233-236. doi: 10.16766/j.cnki.issn.1674-4152.002320 [3] ROQUILLY A, MOYER J D, HUET O, et al. Effect of continuous infusion of hypertonic saline vs standard care on 6-month neurological outcomes in patients with traumatic brain injury: the cobi randomized clinical trial[J]. JAMA, 2021, 325(20): 2056-2066. doi: 10.1001/jama.2021.5561 [4] SCHIFF N D, GIACINO J T, BUTSON C R, et al. Thalamic deep brain stimulation in traumatic brain injury: a phase 1, randomized feasibility study[J]. Nat Med, 2023, 29(12): 3162-3174. doi: 10.1038/s41591-023-02638-4 [5] YUAN H L, LIU B, LI F Z, et al. Effects of intermittent theta-burst transcranial magnetic stimulation on post-traumatic stress disorder symptoms: a randomized controlled trial[J]. Psychiatry Res, 2023, 329: 115533. DOI: 10.1016/j.psychres.2023.115533. [6] KUIPER H, VAN LEEUWEN C C M, KOPSKY D J, et al. Post-traumatic stress disorder symptoms and pain intensity in persons with spinal cord injury[J]. Spinal Cord, 2021, 59(3): 328-335. doi: 10.1038/s41393-020-00599-w [7] 严雯婕, 张海燕, 程素慧, 等. 创伤后应激障碍的共病及机制[J]. 海军军医大学学报, 2024, 45(5): 634-639.YAN W J, ZHANG H Y, CHENG S H, et al. Comorbidities and mechanisms of post-traumatic stress disorder[J]. Academic Journal of Naval Medical University, 2024, 45(5): 634-639. [8] 贺亚龙, 刘文博. 颅脑创伤后加重继发性脑损伤的危险因素防治专家共识[J]. 临床神经外科杂志, 2020, 17(3): 241-249, 253.HE Y L, LIU W B. Experts Consensus on the management of factors of secondary brain insults following traumatic brain injury[J]. Journal of Clinical Neurosurgery, 2020, 17(3): 241-249, 253. [9] SOLDATOS C R, DIKEOS D G, PAPARRIGOPOULOS T J. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria[J]. J Psychosom Res, 2000, 48(6): 555-560. doi: 10.1016/S0022-3999(00)00095-7 [10] 耿亚琴, 许勤, 刘惠贤, 等. 中文版创伤后成长量表在多发伤幸存者中应用的信效度分析[J]. 中华护理杂志, 2011, 46(10): 1003-1005.GENG Y Q, XU Q, LIU H X, et al. Reliability and validity analysis of the Chinese version of post-traumatic Growth Scale in multiple injury survivors[J]. Chinese Journal of Nursing, 2011, 46(10): 1003-1005. [11] HOU W K, LAM W W T, LAW C C, et al. Measuring social relational quality in colorectal cancer: the Social Relational Quality Scale(SRQS)[J]. Psychooncology, 2009, 18(10): 1097-1105. doi: 10.1002/pon.1500 [12] 刘贤臣, 马登岱, 刘连启, 等. 心理创伤后应激障碍自评量表的编制和信度效度研究[J]. 中国行为医学科学, 1998(2): 14-17.LIU X C, MA D D, LIU L Q, et al. Development of the post-traumatic stress disorder self-rating sca leand its reliability and validity[J]. Chinese Journal of Behavioral Medical Science, 1998(2): 14-17. [13] GITAARI M, MIKOLIC A, PANENKA W J, et al. Diagnostic accuracy of mental health screening tools after mild traumatic brain injury[J]. JAMA Netw Open, 2024, 7(7): e2424076. DOI: 10.1001/jamanetworkopen.2024.24076. [14] 刘强, 秦燕. 正念减压训练对交通事故幸存者创伤后应激障碍的干预效果[J]. 第三军医大学学报, 2021, 43(7): 663-669.LIU Q, QIN Y. Intervention effects of mindfulness-based stress reduction training on post-traumatic stress disorder in traffic accident survivorsJ]. Journal of Third Military Medical University, 2021, 43(7): 663-669. [15] 陈晓倩, 张希萍, 黄赣英, 等. 老年车祸多发伤患者创伤后应激障碍的影响因素及相关对策[J]. 武汉大学学报(医学版), 2024, 45(3): 335-338, 372.CHEN X Q, ZHANG X P, HUANG G Y, et al. Influencing factors and related countermeasures of post?traumatic stress disorder in elderly patients with multiple injuries in car accidents[J]. Medical Journal of Wuhan University, 2024, 45(3): 335-338, 372. [16] 史姝, 史林飞. 脑卒中合并创伤后应激障碍的危险因素探讨及风险列线图模型的建立[J]. 中西医结合心脑血管病杂志, 2021, 19(10): 1734-1738.SHI S, SHI L F. Study on risk factors of stroke complicated with post-traumatic stress disorder and establishment of risk nomogram model[J]. Chinese Journal of Integrative Medicine on Cardio-Cerebrovascular Disease, 2021, 19(10): 1734-1738. [17] 魏乐, 张伟, 如克亚·白克力. 重型颅脑损伤病人创伤后应激障碍的风险因素分析[J]. 中国临床神经外科杂志, 2023, 28(2): 92-95.WEI L, ZHANG W, RUKEA BAIKELIL. Risk factors for post-traumatic stress disorder in patients with severe traumatic brain injury[J]. Chinese Journal of Clinical Neurosurgery, 2023, 28(2): 92-95. [18] 王松青, 杨华, 黄仁强, 等. 颅脑损伤相关创伤后应激障碍的影响因素分析[J]. 中华神经外科疾病研究杂志, 2024, 18(1): 21-26.WANG S Q, YANG H, HUANG R Q, et al. Analysis of influencing factors of post-traumatic stress disorder associated with traumatic brain injury[J]. Chinese Journal of Neurosurgical Disease Research, 2024, 18(1): 21-26. [19] ANSBJERG M B, SANDAHL H, BAANDRUP L, et al. Sleep impairments in refugees diagnosed with post-traumatic stress disorder: a polysomnographic and self-report study[J]. Eur Psychotraumatol, 2023, 14(1): 2185943. DOI: 10.1080/20008066.2023.2185943. [20] 王丽萍. 颅脑损伤患者术后创伤后成长与创伤后应激障碍的相关性[J]. 中国实用神经疾病杂志, 2021, 24(4): 352-356.WANG L P. Correlation between post-traumatic growth and post-traumatic stress disorder in patients with brain injury[J]. Chinese Journal of Practical Nervous Diseases, 2021, 24(4): 352-356. [21] GORMAN I, BELSER A B, JEROME L, et al. Posttraumatic growth after MDMA-Assisted psychotherapy for posttraumatic stress disorder[J]. J Trauma Stress, 2020, 33(2): 161-170. doi: 10.1002/jts.22479 [22] LUO M X, EDELSBRUNNER P A, SIEBERT J S, et al. Longitudinal within-person associations between quality of social relations, structure of social relations, and cognitive functioning in older age[J]. J Gerontol B Psychol Sci Soc Sci, 2021, 76(10): 1960-1971. doi: 10.1093/geronb/gbab001 [23] 付爽, 刘祯, 崔玉顺. 中青年首发脑卒中患者心理一致感在领悟社会支持与创伤后应激障碍的中介效应[J]. 护理学报, 2023, 30(20): 43-47.FU S, LIU Z, CUI Y S. The mediating effect of psychological congruence on understanding social support and post-traumatic stress disorder in young and middle-aged patients with first-episode stroke[J]. Journal of Nursing(China), 2023, 30(20): 43-47. [24] 高俊, 陈晓敏, 马静, 等. 早期认知行为干预对颅脑损伤患者的干预效果及心理应激水平的影响[J]. 河北医药, 2024, 46(18): 2870-2873.GAO J, CHEN X M, MA J, et al. Effect of early cognitive behavioral intervention on psychological stress in patients with craniocerebral injury[J]. Hebei Medical Journal, 2024, 46(18): 2870-2873. -





 下载:
下载: