Serum levels of C1q/TNF-related protein 9 and its association with insulin resistance in gestational diabetes mellitus
-
摘要:
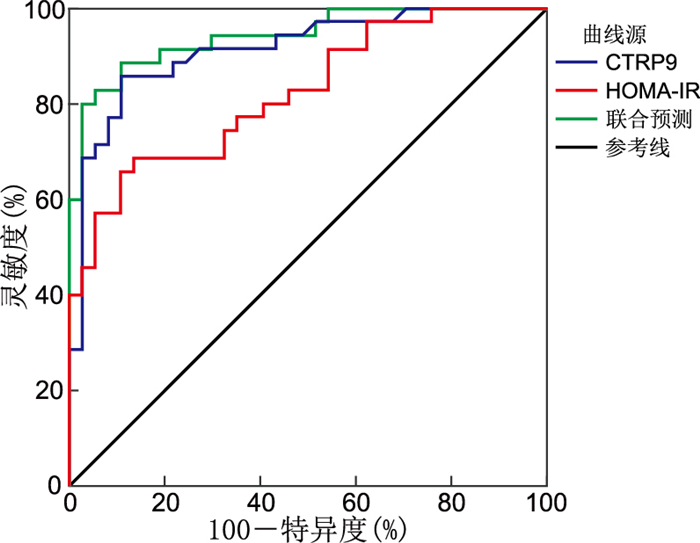
目的 探讨妊娠期糖尿病(GDM)孕妇血清C1q/肿瘤坏死因子相关蛋白9(CTRP9)的表达水平及其应用价值。 方法 选取2019年10月—2020年10月在淮安市第一人民医院就诊的35名GDM患者(GDM组)和37名健康孕妇(对照组)。比较2组孕妇的一般资料、糖代谢指标、CTRP9及其他脂肪因子水平,并通过Pearson相关分析研究脂肪因子与GDM患者临床指标的相关性。 结果 GDM组空腹血糖(FPG)、口服葡萄糖耐量试验(OGTT)1 h血糖(1hPG)、2 h血糖(2hPG)、空腹胰岛素(FINS)、稳态模型胰岛素抵抗指数(HOMA-IR)、白介素-6(IL-6)、瘦素(leptin)、肿瘤坏死因子-α(TNF-α)、CTRP9水平均高于正常对照组(P<0.05)。Pearson相关分析显示:血清CTRP9与FPG、1hPG、2hPG、FINS、HOMA-IR、IL-6和TNF-α均呈正相关关系(P<0.05)。Logistic回归分析显示升高的HOMA-IR(OR=14.771, P=0.046)和CTRP9(OR=4.965, P=0.002)是GDM发生的独立危险因素。ROC分析显示,CTRP9、HOMA-IR诊断GDM的曲线下面积分别为0.914和0.822;二者联合检测的曲线下面积为0.943,诊断效能最佳。 结论 GDM孕妇血清中CTRP9水平升高,CTRP9升高是GDM发生的独立危险因素。CTRP9联合HOMA-IR筛查GDM的价值优于单一指标。 -
关键词:
- 妊娠期糖尿病 /
- C1q/肿瘤坏死因子相关蛋白9 /
- 脂肪因子 /
- 胰岛素抵抗
Abstract:Objective To investigate the relationship between serum C1q/tumor necrosis factor-related protein 9 (CTRP9) and gestational diabetes mellitus (GDM) and its clinical significance. Methods A total of 35 patients with GDM and 37 pregnant women without the condition were enrolled. The general characteristics, glucose metabolism indicators, serum CTRP9 levels and other adipokine levels were compared between the two groups. In addition, a Pearson correlation analysis was conducted to examine the correlation between serum CTRP9, other cytokines and clinical indexes in pregnant women with GDM. Results The fasting plasma glucose (FPG), OGTT 1hPG, OGTT 2hPG, fasting insulin (FINS), HOMA-IR, interleukin-6 (IL-6), leptin, tumor necrosis factor-α (TNF-α), and CTRP9 in the GDM group were higher than those in the control group (P<0.05). The results of the Pearson correlation analysis indicated that serum CTRP9 was positively correlated with FPG, 1hPG, 2hPG, FINS, HOMA-IR, IL-6 and TNF-α (P<0.05). The logistic regression analysis showed that elevated HOMA-IR (OR=14.771, P=0.046) and CTRP9 (OR=4.965, P=0.002) were independent risk factors for GDM. ROC analysis demonstrated that CTRP9 and HOMA-IR had areas under the curve of 0.914 and 0.822, respectively, for diagnosing GDM. The combined detection had an area under the curve of 0.943, indicating optimal diagnostic efficiency. Conclusion The serum CTRP9 level is elevated in GDM. Elevated serum CTRP9 level is an independent risk factor for GDM. Furthermore, the combination of serum CTRP9 and HOMA-IR was more efficient in screening for GDM. -
表 1 对照组和GDM组孕妇一般临床资料、血糖代谢指标及脂肪因子比较
Table 1. Comparison of general clinical data, blood glucose metabolism indexes and adipokines between the control group and the GDM group
项目 对照组(n=37) GDM组(n=35) 统计量 P值 年龄(x±s,岁) 30.43±4.53 31.26±5.65 -0.685a 0.495 孕周[M(P25, P75),周] 25.00(23.43,25.57) 25.43(24.00,27.57) -1.259b 0.208 BMI(x±s) 26.48±3.66 26.50±3.62 -0.019a 0.985 SBP(x±s,mmHg) 111.57±9.80 114.80±10.60 -1.344a 0.183 DBP(x±s,mmHg) 65.97±7.96 67.80±7.94 -0.975a 0.333 FPG(x±s,mmol/L) 3.94±0.32 4.90±0.89 -6.014a <0.001 1hPG(x±s,mmol/L) 6.50±0.99 9.79±1.15 -13.003a <0.001 2hPG(x±s,mmol/L) 5.88±0.80 8.14±1.52 -7.797a <0.001 FINS(x±s,pmol/L) 6.63±2.29 9.09±3.01 -3.912a <0.001 HOMA-IR(x±s) 1.17±0.44 2.01±0.89 -5.083a <0.001 ALT(x±s,U/L) 15.14±4.60 14.69±4.14 0.443a 0.659 AST[M(P25, P75),U/L] 16.30(14.60,18.90) 15.70(13.20,18.00) -0.896b 0.370 TC(x±s,mmol/L) 5.46±0.87 5.17±0.86 1.395a 0.167 HDL-C(x±s,mmol/L) 1.83±0.36 1.85±0.45 -0.216a 0.829 LDL-C(x±s,mmol/L) 3.17±0.82 2.89±0.94 1.377a 0.173 TG[M(P25, P75),mmol/L] 2.35(1.81,2.79) 2.17(1.87,3.22) -0.524b 0.600 Scr(x±s,μmol/L) 44.62±4.88 45.00±5.53 -0.308a 0.759 UA(x±s,μmol/L) 207.84±47.87 216.80±34.86 -0.904a 0.369 NEUT(x±s,×109/L) 6.59±1.34 6.94±1.51 -1.046a 0.299 IL-6(x±s,pg/mL) 0.28±0.10 0.50±0.29 -4.241a <0.001 Leptin[M(P25, P75),μg/L] 4.68(2.98,6.83) 6.83(3.73,10.21) -2.682b 0.007 MCP-1(x±s,pg/mL) 86.65±21.41 77.48±20.03 1.873a 0.065 TNF-α[M(P25, P75),pg/mL] 0.56(0.35,0.85) 0.84(0.68,1.19) -3.793b <0.001 IL-1β[M(P25, P75),pg/mL] 0.23(0.19,0.31) 0.21(0.16,0.26) -1.808b 0.071 CTRP9(x±s,pg/mL) 1.27±0.67 3.07±1.15 -8.055a <0.001 注:a为t值,b为Z值。1 mmHg=0.133 kPa。 表 2 影响GDM发生的二元logistic回归分析
Table 2. Binary logistic regression analysis of the occurrence of GDM
影响因素 B SE Waldχ2 P值 OR值(95% CI) HOMA-IR 2.693 1.346 3.999 0.046 14.771(1.055~206.793) IL-6 4.965 3.319 2.238 0.135 143.378(0.215~95 837.333) TNF-α 3.007 1.622 3.439 0.064 20.235(0.843~485.868) CTRP9 1.602 0.514 9.733 0.002 4.965(1.814~13.588) -
[1] 中华医学会妇产科学分会产科学组, 中华医学会围产医学分会, 中国妇幼保健协会妊娠合并糖尿病专业委员会. 妊娠期高血糖诊治指南(2022)[第二部分][J]. 中华妇产科杂志, 2022, 57(2): 81-90. https://www.cnki.com.cn/Article/CJFDTOTAL-GWVC202206020.htmChinese Society of Obstetrics and Gynecology, Chinese Society of Perinatal Medicine, Professional Committee of Gestational Diabetes Mellitus, Chinese Maternal and Child Health Association. Guideline of diagnosis and treatment of hyperglycemia in pregnancy(2022)[Part two][J]. Chinese Journal of Obstetrics and Gynecology, 2022, 57(2): 81-90. https://www.cnki.com.cn/Article/CJFDTOTAL-GWVC202206020.htm [2] NERI C, SERAFINO E, MORLANDO M, et al. Microbiome and gestational diabetes: interactions with pregnancy outcome and long-term infant health[J]. J Diabetes Res, 2021, 2021: 9994734. DOI: 10.1155/2021/9994734. [3] MOON J H, JANG H C. Gestational diabetes mellitus: diagnostic approaches and maternal-offspring complications[J]. Diabetes Metab J, 2022, 46(1): 3-14. doi: 10.4093/dmj.2021.0335 [4] XU X, HUANG F P, GUO Y N, et al. Interactive effect of prepregnancy overweight/obesity and GDM history on prevalence of GDM in biparous women[J]. Front Endocrinol (Lausanne), 2023, 14: 1084288. DOI: 10.3389/fendo.2023.1084288. [5] ŠIMJÁK P, CINKAJZLOVÁ A, ANDERLOVÁ K, et al. The role of obesity and adipose tissue dysfunction in gestational diabetes mellitus[J]. J Endocrinol, 2018, 238(2): R63-R77. doi: 10.1530/JOE-18-0032 [6] XIA L, ZHANG H J, SHI Q, et al. Protective role of CTRP3 and CTRP9 in the development of gestational diabetes mellitus[J]. Clin Lab, 2020, 66(11). DOI: 10.7754/Clin.Lab.2020.200247. [7] NA N, JI M. Role of first-trimester serum C1q/TNF-related protein 9 in gestational diabetes mellitus[J]. Clin Lab, 2020, 66(12). DOI: 10.7754/Clin.Lab.2020.200434. [8] JUAN J, YANG H X. Prevalence, prevention, and lifestyle intervention of gestational diabetes mellitus in China[J]. Int J Environ Res Public Health, 2020, 17(24): 9517. DOI: 10.3390/ijerph17249517. [9] CHO N H, SHAW J E, KARURANGA S, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045[J]. Diabetes Res Clin Pract, 2018, 138: 271-281. doi: 10.1016/j.diabres.2018.02.023 [10] 林苗, 周平. 妊娠期糖尿病孕妇产后高血糖的危险因素分析[J]. 中华全科医学, 2022, 20(8): 1350-1352, 1356. doi: 10.16766/j.cnki.issn.1674-4152.002594LIN M, ZHOU P. Risk factors of postpartum hyperglycaemia in pregnant women with gestational diabetes mellitus[J]. Chinese Journal of General Practice, 2022, 20(8): 1350-1352, 1356. doi: 10.16766/j.cnki.issn.1674-4152.002594 [11] ZUO A J, ZHAO X Y, LI T T, et al. CTRP9 knockout exaggerates lipotoxicity in cardiac myocytes and high-fat diet-induced cardiac hypertrophy through inhibiting the LKB1/AMPK pathway[J]. J Cell Mol Med, 2020, 24(4): 2635-2647. doi: 10.1111/jcmm.14982 [12] 何新梅, 陈丹青. 妊娠期糖尿病孕妇血清CTRP6水平及意义[J]. 中华全科医学, 2020, 18(10): 1699-1701. doi: 10.16766/j.cnki.issn.1674-4152.001597HE X M, CHEN D Q. Serum CTRP6 level in pregnant women with diabetes during pregnancy and its significance[J]. Chinese Journal of General Practice, 2020, 20(8): 1699-1701. doi: 10.16766/j.cnki.issn.1674-4152.001597 [13] ZAIDI H, BYRKJELAND R, NJERVE I U, et al. Adiponectin in relation to exercise and physical performance in patients with type 2 diabetes and coronary artery disease[J]. Adipocyte, 2021, 10(1): 612-620. doi: 10.1080/21623945.2021.1996699 [14] BOZZETTO L, POLITO R, NIGRO E, et al. Dietary influence on adiponectin in patients with type 2 diabetes[J]. Eur J Clin Invest, 2021, 51(8): e13548. DOI: 10.1111/eci.13548. [15] NOMURA H, ARASHI H, YAMAGUCHI J, et al. Relation of adiponectin to cardiovascular events and mortality in patients with acute coronary syndrome[J]. Am J Cardiol, 2021, 140: 7-12. doi: 10.1016/j.amjcard.2020.10.053 [16] LI L, GU Z Y, ZHANG J J. CTRP9 overexpression attenuates palmitic acid-induced inflammation, apoptosis and impaired migration in HTR8/SVneo cells through AMPK/SREBP1c signaling[J]. Exp Ther Med, 2022, 24(1): 459. doi: 10.3892/etm.2022.11386 [17] MORADI N, FADAEI R, EMAMGHOLIPOUR S, et al. Association of circulating CTRP9 with soluble adhesion molecules and inflammatory markers in patients with type 2 diabetes mellitus and coronary artery disease[J]. PLoS One, 2018, 13(1): e0192159. DOI: 10.1371/journal.pone.0192159. [18] LACROIX M, LIZOTTE F, HIVERT M F, et al. Calcifediol decreases interleukin-6 secretion by cultured human trophoblasts from GDM pregnancies[J]. J Endocr Soc, 2019, 3(11): 2165-2178. doi: 10.1210/js.2019-00181 [19] AMIRIAN A, MAHANI M B, ABDI F. Role of interleukin-6 (IL-6) in predicting gestational diabetes mellitus[J]. Obstet Gynecol Sci, 2020, 63(4): 407-416. doi: 10.5468/ogs.20020 [20] RUSZALA M, NIEBRZYDOWSKA M, PILSZYK A, et al. Novel biomolecules in the pathogenesis of gestational diabetes mellitus[J]. Int J Mol Sci, 2021, 22(21): 11578. DOI: 10.3390/ijms222111578. -





 下载:
下载: