Correlation between multiple chronic conditions and long-term heart failure after acute myocardial infarction
-
摘要:
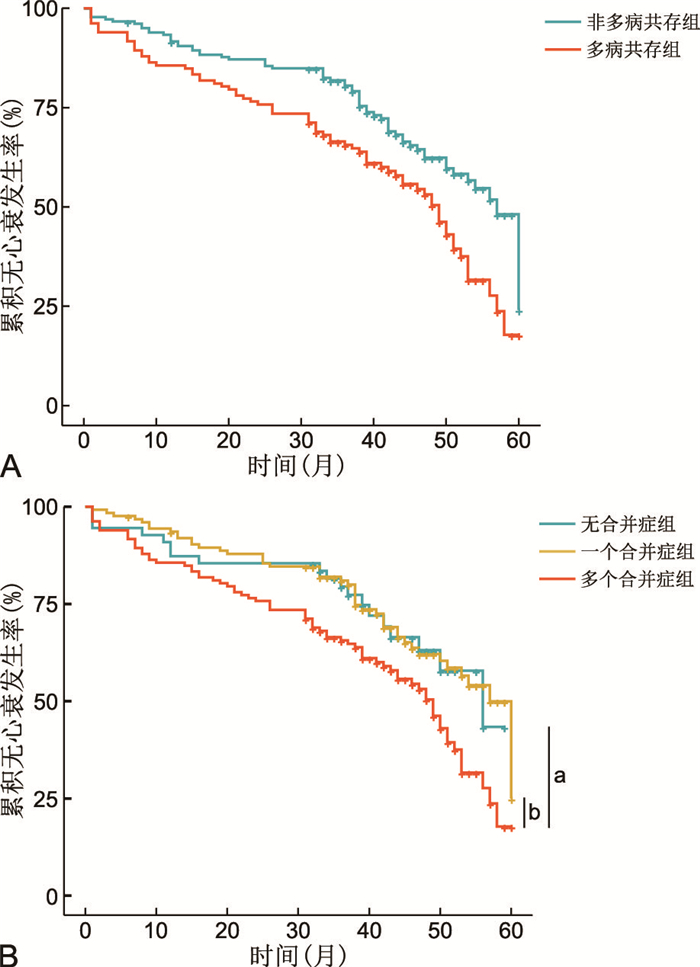
目的 分析急性心肌梗死(AMI)患者远期心力衰竭(HF)的发生情况,并探讨多病共存(MCC)与其相关性。 方法 选择2016年1月—2018年12月在扬州大学附属医院心内科住院的AMI患者355例,根据结局分为心衰组(149例)和非心衰组(206例),中位随访时间为43.0个月。回顾性分析2组患者的基线资料;使用Kaplan-Meier分析和Cox回归分析评估MCC在AMI患者远期HF发生中的作用;运用Cochran-Armitage检验分析共存疾病数与AMI患者远期HF发生率的关系。 结果 (1) 心衰组患者年龄更大,左心室射血分数更低,GRACE评分及MCC占比更高。心衰组MCC发生率为非心衰组的1.6倍;(2)年龄(HR=1.024,95% CI: 1.003~1.045)、低左室射血分数(HR=0.963,95% CI: 0.946~0.980)、GRACE评分(HR=1.011,95% CI: 1.004~1.018)及MCC(HR=1.517,95% CI: 1.073~2.146)是AMI患者远期HF的独立影响因素;(3)MCC患者AMI后远期HF的发生率明显高于非MCC患者(P<0.05);(4)AMI患者远期HF发生率与共存疾病数呈正相关关系(P<0.05)。 结论 MCC是AMI患者远期HF的独立危险因素,对AMI患者远期HF的发生具有预测价值,且远期HF发生率随共存疾病数的增加而增高。 Abstract:Objective To analyze the incidence of long-term heart failure (HF) in patients with acute myocardial infarction (AMI), and explore the correlation between multiple chronic conditions (MCC) with it. Methods An analysis was performed on 355 patients with AMI hospitalized in the Department of Cardiology of Affiliated Hospital of Yangzhou University from January 2016 to December 2018. Patients were divided into HF group (149 cases) and non-HF group (206 cases) according to the outcome, with a median follow-up of 43.0 months. The baseline data of the two groups were retrospectively analyzed. Kaplan-Meier analysis and Cox regression analysis were used to evaluate the role of MCC in long-term HF in patients with AMI. The Cochran-Armitage trend test was used to analysis the relationship between the number of coexisting diseases and the incidence of long-term HF in AMI patients. Results (1) Patients in the HF group were older, with lower left ventricular ejection fraction, and had higher GRACE scores and proportion of MCC. The proportion of MCC in the HF group was 1.6 times higher than that in the non-HF group. (2) Age (HR=1.024, 95% CI: 1.003-1.045), low left ventricular ejection fraction (HR=0.963, 95% CI: 0.946-0.980), GRACE scores (HR=1.011, 95% CI: 1.004-1.018) and MCC (HR=1.517, 95% CI: 1.073-2.146) were independent influence factors for long-term HF in AMI patients. (3) The cumulative incidence of HF after AMI was significantly higher in patients with MCC than that in patients without MCC (P < 0.05). (4) There was a positive correlation between the incidence of distant HF and the number of coexisting diseases in AMI patients (P < 0.05). Conclusion MCC is an independent risk factor for long-term HF in patients with AMI, which has predictive value for the occurrence of long-term HF in AMI patients, and the incidence of long-term HF after AMI increases with the number of coexisting diseases. -
表 1 心衰组与非心衰组患者临床资料比较
Table 1. Comparison of clinical data between HF group and non-HF group
项目 非心衰组(n=206) 心衰组(n=149) 统计量 P值 人口学特征 年龄[M(P25, P75),岁] 60.0(51.0, 67.0) 70.0(61.0, 76.5) -6.361a < 0.001 性别(男性/女性,例) 169/37 113/36 2.035b 0.154 临床特征 心率[M(P25, P75),次/min] 72.0(64.8, 80.3) 75.0(66.0, 85.5) -2.321a 0.020 收缩压[M(P25, P75),mmHg] 135.5(120.0, 150.0) 130.0(120.0, 150.0) -1.094a 0.274 舒张压[M(P25, P75),mmHg] 80.0(74.8, 94.3) 80.0(70.0, 90.0) -2.239a 0.025 GRACE评分(x±s) 137.8±31.1 167.2±31.2 8.765c < 0.001 实验室及器械检查 红细胞(x±s,×1012/L) 4.70±0.53 4.60±0.58 -1.707c 0.089 血红蛋白[M(P25, P75),g/L] 147.0(136.8, 157.0) 140.0(130.0, 154.0) -2.815a 0.005 血小板[M(P25, P75),×109/L] 184.5(156.0, 226.0) 178.0(149.5, 213.5) -1.208a 0.227 白细胞[M(P25, P75),×109/L] 8.6(7.3, 10.9) 9.1(7.2, 11.2) -0.920a 0.358 血钾[M(P25, P75),mmol/L] 4.0(3.7, 4.2) 3.9(3.7, 4.3) -0.256a 0.798 白蛋白[M(P25, P75),g/L] 41.7(39.4, 44.5) 40.5(37.5, 44.1) -2.450a 0.014 总胆红素[M(P25, P75),μmol/L] 8.9(4.5, 13.5) 8.1(4.2, 14.7) -0.382a 0.702 谷草转氨酶[M(P25, P75),U/L] 44.0(27.0, 91.3) 45.0(28.9, 92.5) -0.808a 0.419 血糖[M(P25, P75),mmol/L] 7.5(6.1, 10.3) 8.3(6.4, 12.2) -2.077a 0.038 肌酐[M(P25, P75),μmol/L] 72.8(62.0, 85.3) 75.0(63.0, 89.1) -1.362a 0.173 甘油三酯[M(P25, P75),μmol/L] 1.8(1.3, 2.6) 1.4(1.1, 2.0) -4.662a < 0.001 LDL-C[M(P25, P75),mmol/L] 2.3(1.9, 2.8) 2.3(1.9, 2.8) -0.101a 0.919 D二聚体[M(P25, P75),mg/L] 0.2(0.1, 0.4) 0.4(0.2, 0.6) -5.302a < 0.001 LVEF[M(P25, P75),%] 67.0(62.0, 70.0) 61.0(55.0, 67.0) -5.803a < 0.001 既往史[例(%)] 吸烟史 104(50.5) 64(43.0) 1.968b 0.161 高血压史 139(67.5) 114(76.5) 3.446b 0.063 糖尿病史 37(18.0) 48(32.2) 9.646b 0.002 冠心病史 26(12.6) 36(24.2) 7.988b 0.005 脑卒中史 20(9.7) 30(20.1) 7.766b 0.005 高脂血症史 20(9.7) 7(4.7) 3.089b 0.079 MCC 66(32.0) 78(52.3) 14.793b < 0.001 院内治疗 PCI治疗[例(%)] 177(85.9) 115(77.2) 4.526b 0.003 注:a为Z值,b为χ2值, c为t值。LDL-C为低密度脂蛋白胆固醇。1 mmHg=0.133 kPa。 表 2 AMI患者远期HF影响因素的单因素Cox回归分析
Table 2. Univariate Cox regression analysis of long-term HF influencing factors in AMI patients
项目 B SE Wald χ2 P值 HR值 95% CI 年龄 0.046 0.007 42.046 <0.001 1.048 1.033~1.062 心率 0.012 0.005 5.218 0.022 1.012 1.002~1.023 舒张压 -0.012 -0.006 4.556 0.033 0.988 0.977~0.999 LVEF -0.052 0.008 42.236 <0.001 0.949 0.934~0.964 血红蛋白 -0.012 0.004 10.706 0.001 0.988 0.981~0.995 白蛋白 -0.051 0.018 7.960 0.005 0.950 0.917~0.984 血糖 0.036 0.017 4.434 0.035 1.036 1.002~1.071 甘油三酯 -0.285 0.085 11.135 0.001 0.752 0.636~0.889 GRACE评分 0.018 0.002 71.379 <0.001 1.018 1.014~1.022 D-二聚体 0.026 0.025 1.121 0.290 1.027 0.978~1.078 PCI治疗 -0.302 0.196 2.384 0.123 0.739 0.504~1.085 冠心病史 0.704 0.193 13.311 <0.001 2.021 1.385~2.950 糖尿病史 0.625 0.176 12.558 <0.001 1.867 1.322~2.638 脑卒中史 0.718 0.207 12.025 0.001 2.049 1.366~3.074 MCC 0.668 0.165 16.376 <0.001 1.950 1.411~2.696 表 3 AMI患者远期HF影响因素的多因素Cox回归分析
Table 3. Multivariate Cox regression analysis of long-term HF influencing factors in AMI patients
项目 B SE Wald χ2 P值 HR值 95% CI 年龄 0.024 0.011 2.268 0.023 1.024 1.003~1.045 心率 0.005 0.006 0.803 0.422 1.005 0.993~1.017 舒张压 0.011 0.007 1.549 0.121 1.011 0.997~1.025 LVEF -0.038 0.009 -4.192 <0.001 0.963 0.946~0.980 血红蛋白 -0.002 0.005 -0.278 0.781 0.998 0.988~1.009 白蛋白 0.013 0.019 0.677 0.499 1.013 0.976~1.050 血糖 0.019 0.019 1.030 0.303 1.019 0.983~1.058 甘油三酯 -0.150 0.089 -1.684 0.092 0.861 0.724~1.025 GRACE评分 0.011 0.004 2.984 0.003 1.011 1.004~1.018 MCC 0.417 0.177 2.358 0.018 1.517 1.073~2.146 -
[1] 娄逸, 钱菊英, 陈章炜, 等. 2型糖尿病对急性STEMI患者经皮冠状动脉介入治疗后炎症反应及远期心肌重构的影响[J]. 中国临床医学, 2019, 26(3): 398-405. https://www.cnki.com.cn/Article/CJFDTOTAL-LCYX201903016.htmLOU Y, QIAN J Y, CHEN Z W, et al. The role of diabetes mellitus in inflammatory reaction and long-term cardiac remodeling in patients diagnosed with acute myocardial infarction underwent primary percutaneous coronary intervention[J]. Chinese Journal of Clinical, 2019, 26(3): 398-405. https://www.cnki.com.cn/Article/CJFDTOTAL-LCYX201903016.htm [2] 中国心血管健康与疾病报告编写组. 中国心血管健康与疾病报告2021概要[J]. 中国循环杂志, 2022, 37(6): 553-578. doi: 10.3969/j.issn.1000-3614.2022.06.001The Writing Committee of the Report on Cardiovascular Health and Diseases in China. Report on Cardiovascular Health and Diseases in China 2021: an Updated Summary[J]. Chinese Circulation Journal, 2022, 37(6): 553-578. doi: 10.3969/j.issn.1000-3614.2022.06.001 [3] SEFEROVIC P M, PIEPOLI M F, LOPATIN Y, et al. Heart Failure Association of the European Society of Cardiology Quality of Care Centres Programme: design and accreditation document[J]. Eur J Heart Fail, 2020, 22(5): 763-774. doi: 10.1002/ejhf.1784 [4] 唐天娇, 曹立, 董碧蓉, 等. 老年人多病共存名词和定义专家共识(2022)[J]. 中华老年医学杂志, 2022, 41(9): 1028-1031. doi: 10.3760/cma.j.issn.0254-9026.2022.09.002TANG T J, CAO L, DONG B R, et al. Chinese expert consensus on the term and definition of multimorbidity in older adults(2022)[J]. Chinese Journal of Geriatrics, 2022, 41(9): 1028-1031. doi: 10.3760/cma.j.issn.0254-9026.2022.09.002 [5] 甘勇, 杨婷婷, 杨宇迪, 等. 基于系统基模的慢性病主要危险因素分析及对策研究[J]. 中华全科医学, 2019, 17(12): 2046-2050, 2054. doi: 10.16766/j.cnki.issn.1674-4152.001124GAN Y, YANG T T, YANG Y D, et al. Analysis of main risk factors and countermeasures of chronic diseases based on systems archetypes[J]. Chinese Journal of General Practice, 2019, 17(12): 2046-2050, 2054. doi: 10.16766/j.cnki.issn.1674-4152.001124 [6] MCMANUS D D, NGUYEN H L, SACZYNSKI J S, et al. Multiple cardiovascular comorbidities and acute myocardial infarction: temporal trends(1990-2007)and impact on death rates at 30 days and 1 year[J]. Clin Epidemiol, 2012, 2012: 115-123. [7] RINKMANN C, SCHOFER J. 4th universal definition of myocardial infarction 2018: what is new?[J]. Herz, 2018, 43(8): 681-688. doi: 10.1007/s00059-018-4763-6 [8] 国家卫生计生委合理用药专家委员会, 中国药师协会. 心力衰竭合理用药指南(第2版)[J]. 中国医学前沿杂志(电子版), 2019, 11(7): 1-78. https://www.cnki.com.cn/Article/CJFDTOTAL-YXQY201907001.htmCommittee of Exports on Rational Drug Use National Health and Family Planning Commission of The People's Republic of China; Chinese Pharmacists Association. Guidelines for rational use of drugs of heart failure(2 edition)[J]. Chinese Journal of the Frontiers of Medical Science(Electronic Version), 2019, 11(7): 1-78. https://www.cnki.com.cn/Article/CJFDTOTAL-YXQY201907001.htm [9] 廖显明, 王晓婕. 我国老年人慢性病共病的现状和应对策略[J]. 应用预防医学, 2022, 28(2): 191-194, 197. https://www.cnki.com.cn/Article/CJFDTOTAL-GXYX202202028.htmLIAO X M, WANG X L. Current situation and coping strategies of chronic comorbidities among the elderly in China[J]. Applied Preventive Medicine, 2022, 28(2): 191-194, 197. https://www.cnki.com.cn/Article/CJFDTOTAL-GXYX202202028.htm [10] ZHANG F Y, WONG C W, CHIU Y D, et al. Prognostic impact of comorbidity measures on outcomes following acute coronary syndrome: a systematic review[J]. Int J clin Pract, 2021, 75(10): e14345-e14345. DOI: 10.1111/ijcp.14345. [11] 严研, 公威, 王晓, 等. 多病共患的老年急性冠状动脉综合征患者抗栓治疗情况及预后分析[J]. 中华心血管病杂志, 2022, 50(5): 443-449.YAN Y, GONG W, WANG X, et al. Multimorbidity in elderly patients with acute coronary syndrome: insights from BleeMACS registry[J]. Chinese Journal of Cardiology, 2022, 50(5): 443-449. [12] LIU G H, XUE Y L, LIU Y H, et al. Multimorbidity in cardiovascular disease and association with life satisfaction: a Chinese national cross-sectional study[J]. BMJ Open, 2020, 10(12): e042950. DOI: 10.1136/BMJopen-2020-042950. [13] BREEN K, FINNEGAN L, VUCKOVIC K, et al. Multimorbidity in patients with acute coronary syndrome is associated with greater mortality, higher readmission rates, and increased length of stay: a systematic review[J]. J Cardiovasc Nurs, 2020, 35(6): E99-E110. DOI: 10.1097/JCN.0000000000000748. [14] HALL M, DONDO T B, YAN A T, et al. Multimorbidity and survival for patients with acute myocardial infarction in England and Wales: latent class analysis of a nationwide population-based cohort[J]. PLos Med, 2018, 15(3): e1002501. DOI: 10.1371/journal.pmed.1002501. [15] 黄萍, 汪铭涵, 张安, 等. 上海实施国家基本公共卫生服务项目十年效果评价[J]. 中华全科医学, 2020, 18(12): 1979-1983. doi: 10.16766/j.cnki.issn.1674-4152.001668HUANG P, WANG M R, ZHANG A, et al. Evaluation of the ten-year effect of implementing national basic public health services in Shanghai[J]. Chinese Journal of General Practice, 2020, 18(12): 1979-1983. doi: 10.16766/j.cnki.issn.1674-4152.001668 [16] 胡月, 王雪莲. 高血压患者对家庭医生签约服务利用及效果评价[J]. 卫生软科学, 2019, 33(6): 53-57. https://www.cnki.com.cn/Article/CJFDTOTAL-WRKX201906011.htmHU Y, WANG X L. Study on the utilization and effect evaluation of family doctors' contract service in hypertensive[J]. Soft Science of Health, 2019, 33(6): 53-57. https://www.cnki.com.cn/Article/CJFDTOTAL-WRKX201906011.htm [17] 赖国彬. 全科医疗模式在照顾社区老年多病共存患者中的应用[J]. 中国社区医师, 2021, 37(11): 25-26. https://www.cnki.com.cn/Article/CJFDTOTAL-XCYS202111011.htmLAI G B. Application of general practice model in caring for elderly patients with multiple diseases in the community[J]. Chinese Community Doctors, 2021, 37(11): 25-26. https://www.cnki.com.cn/Article/CJFDTOTAL-XCYS202111011.htm -





 下载:
下载: